The Thyroid Highway: How Your Brain, Gut, Hormones, and Immune System Are All Connected
May 27, 2025
In part I of the thyroid series, I went over what the thyroid is, what it does, some common symptoms of thyroid imbalance, what could be causing the thyroid imbalances, and how the gut is involved. In part II, we are going to dive a little bit deeper.
When we think about thyroid health, we often zero in on the gland itself—but the thyroid doesn’t function in isolation. It’s deeply intertwined with multiple systems in the body, from the pineal gland’s influence on circadian rhythms and melatonin to the pancreas’s role in blood sugar regulation, the gut’s impact on hormone detox, reproductive health, and immune resilience. This intricate web means that symptoms like fatigue, weight gain, fertility struggles, or frequent illness may not start with the thyroid—but they certainly end up there. In this post, we’ll take a holistic tour of the thyroid’s many connections, revealing why true healing often begins upstream.
The Pineal Gland & The Thyroid
The pineal gland is a small, pea-shaped endocrine gland located deep in the center of the brain, often referred to as the “third eye” due to its role in regulating circadian rhythms through the secretion of melatonin. The pineal gland is also recognized not only for its influence on sleep-wake cycles but also for its broader impact on hormonal balance, including its relationship with the thyroid.
Melatonin production, which is closely tied to light exposure and sleep quality, directly affects the hypothalamic-pituitary-thyroid (HPT) axis. Poor melatonin signaling can disrupt thyroid-stimulating hormone (TSH) rhythms and reduce the body’s ability to convert inactive T4 into active T3, leading to symptoms of thyroid dysfunction.
Additionally, chronic stress, blue light exposure at night, and environmental toxins like fluoride can impair pineal gland function, compounding thyroid imbalances. Supporting pineal health through proper sleep hygiene, light exposure, and detoxification can be a critical component of restoring thyroid function from a root-cause perspective.
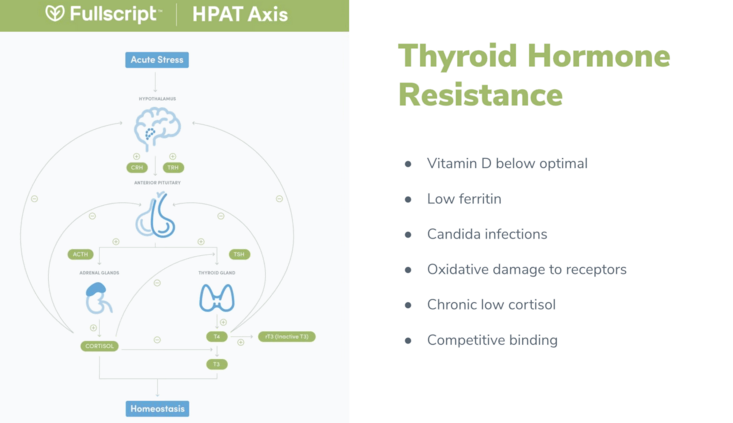
Lastly, the HPAT axis—short for Hypothalamus-Pituitary-Adrenal-Thyroid axis—is a key regulatory network that governs the body’s stress response, hormonal balance, and thyroid function. When someone experiences chronic stress, the hypothalamus and pituitary may shift signals toward cortisol production (via the adrenals), often at the expense of optimal thyroid hormone output. This means thyroid symptoms might actually be a downstream effect of dysfunction higher up in the axis. That’s why it’s essential to look upstream—at the brain and adrenal input—when evaluating thyroid issues, rather than focusing solely on the thyroid gland itself.
The Thyroid-Gut-Hormone-Blood Sugar Connection
The pancreas is attached to the small intestine and sits behind the stomach and helps to produce enzymes that help to digest food (particularly protein) and makes the hormone insulin, which helps to control blood sugar levels.
What most people don’t realize is the pancreas and gut are intricately connected in maintaining metabolic and endocrine balance, and any dysfunction in this axis can significantly impact thyroid health. The pancreas plays a key role in regulating blood sugar through insulin and glucagon, and when gut health is compromised—due to dysbiosis, leaky gut, or chronic inflammation—it can lead to insulin resistance and systemic inflammation.
These imbalances often increase circulating toxins and alter gut-derived hormone signals such as GLP-1 and GIP, which not only affect pancreatic function but also disrupt the hypothalamic-pituitary-thyroid (HPT) axis. Additionally, impaired detoxification through the gut can lead to the reabsorption of estrogens and other hormone-disrupting toxins, placing an added burden on the liver and leading to a buildup of thyroid-disrupting compounds like lipopolysaccharides (LPS).
Over time, this toxic and hormonal stress can suppress thyroid hormone conversion (T4 to T3), trigger autoimmune responses (such as Hashimoto’s thyroiditis), and ultimately impair thyroid function.
Thryoid’s Connection to Reproduction and Infertility
Thyroid health is deeply connected to the function of our reproductive organs, as thyroid hormones help regulate the balance of sex hormones like estrogen, progesterone, and testosterone. When the thyroid is underactive (hypothyroidism), it can disrupt the hormonal signals between the brain and the ovaries or testes, leading to irregular menstrual cycles, PMS, fertility struggles, low libido, or symptoms of estrogen dominance. This is because thyroid hormones influence ovulation, the thickness of the uterine lining, and even how well the body clears out excess hormones.
Additionally, a sluggish thyroid can slow liver detoxification, causing estrogen to recirculate rather than be eliminated properly. The result is hormonal imbalance, which can negatively impact reproductive health and overall vitality. Supporting thyroid function is therefore essential not just for energy and metabolism, but also for healthy, balanced reproductive hormones.
Thyroid- Our Secret Immune Hero
The immune system is the body’s defense against toxins and pathogens including viruses, bacteria, mold, chemicals, metals, and parasites. Some of the main organs involved in the immune system are the spleen, lymph nodes, thymus, and bone marrow.
When we encounter antigens that cause illness, the immune system detects an intruder, sends out a warning message that the body is in danger, and then the immune system directs the specific attacking cells to the problem area to destroy the invaders. When this happens, there is an increase in the production of proteins called antibodies that help to fight off antigens.
When the immune system is stressed, it can manifest as:
- Frequently getting sick
- Increased food and environmental sensitivities
- Autoimmune issues
- Swollen lymph nodes
- Weakness
- Bloating
- Poor Stamina
- Fatigue
- Digestive Issues
The thyroid and immune system have a complex, bidirectional relationship. When there are changes in thyroid hormone levels, the immune cell function and immune system can develop issues that can lead to thyroid dysfunction. Thyroid hormones, such as T3 and T4, can directly influence the behavior and function of immune cells, affecting inflammation, cytokine production, and other immune responses. Conversely, autoimmune diseases like Hashimoto’s thyroiditis and Graves’ disease are examples of immune system errors that attack the thyroid gland, leading to thyroid dysfunction.
The Essential Thyroid Nutrient
A low-functioning thyroid, or hypothyroidism, can make you more susceptible to getting sick often due to its central role in immune regulation and detoxification. The thyroid gland uses iodine to produce hormones and plays a key role in filtering out environmental toxins. However, when the thyroid is underactive, this detoxification process slows down, allowing more toxins to accumulate in the body.
These toxins can deplete selenium, a crucial mineral required not only for thyroid hormone activation but also for strong immune defense. Without adequate selenium, both thyroid function and immune resilience suffer, creating a vicious cycle—low thyroid function leads to poor detoxification, which weakens immunity, making the body more vulnerable to infections and further taxing the thyroid. Supporting the thyroid with nutrients like iodine and selenium is vital to break this cycle and restore immune balance.
Healing the Thyroid Holistically
Thyroid health is far more than just a matter of TSH levels or taking the right medication—it’s a reflection of the body’s overall balance and communication between key systems like the brain, gut, pancreas, reproductive organs, and immune defenses. When one of these systems is out of sync, the thyroid often bears the burden. By taking a root-cause, systems-based approach—supporting melatonin production, balancing blood sugar, optimizing gut health, managing stress, and nourishing the body with key nutrients—we can begin to restore harmony not just to the thyroid, but to the entire body. Your thyroid is not broken; it’s responding to the signals it’s receiving. Let’s work on sending it the right ones!
Schedule your free consultation with me today so that we can work together to get to the root cause of what’s causing your thyroid imbalances and restore the balance.